Often, policymakers want answers to questions like how does the repeal of the Affordable Care Act affect children who have terminal illness? In answering those questions, health insurance claims data represent a good source of information that help public health researchers answer those questions. However, many questions arise about what health insurance claims data is and where it comes from.
What is health insurance claims data? Where does it come from?
Anytime, anyone uses medical care and part of the cost is covered by health insurance, then the insurance company receives a claim for reimbursement that comes from the medical care provider. Looking across a group of individuals such a terminally ill children and following the claims they make over time help researchers answer questions raised by policymakers. However, despite the detailed information that results from millions of medical encounters recorded each day, public health researchers still are hesitant to use claims data.
Why are researchers hesitant to use claims data?
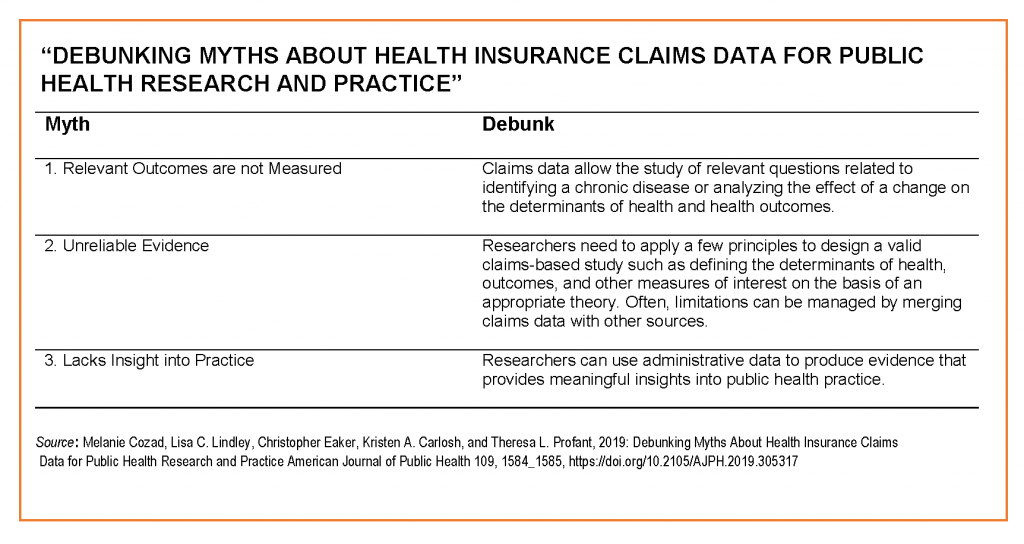
Researchers are hesitant because common myths about the relevance and quality of the data exist. For example, one myth is that claims data don’t measure relevant outcomes for public health. One way to improve public health is to generate evidence about how the effect of an intervention, program, or policy affects health outcomes. Often, researchers believe that claims data lacks relevant outcomes, but in many cases relevant outcomes include mortality, morbidity, prevalence of disease, and costs. These outcomes exist in claims and can offer important insights when research is conducted using data that spans multiple years. Even when relevant outcomes exists, researchers still are reluctant to use claims and ask questions about how reliable the evidence is.
But, isn’t evidence from claims data unreliable?
All data carries limitations and claims data is no exception. A recent white paper by Optum provides a nice description of the scope and advantages of claims data, and highlights its limitations. In addition to limitations of claims data, what is often not well explained is that generation of reliable evidence comes from carefully designing studies to address the data’s limitations. When limitations in the data cannot be addressed through study design being transparent to outline how those limitations affect the conclusions presented is a necessity. Yet, even when researchers feel the evidence generated by using claims data is reliable questions often emerge regarding whether the evidence can provide insights into public practice.
Can evidence from claims data really provide insight into public practice?
As it turns out understanding the impact of policy and predicting future changes in policy’s influence is an important tool for public health practitioners so they can respond appropriately. Researchers used claims data to demonstrate that hospice and home health services were often underutilized by children at the end of life in California. This work paved the way for the inclusion of a concurrent care provision within the Affordable Care Act. Concurrent care enables curative and palliative care therapies to be administered simultaneously. Thus evidence from claims data highlights to policymakers the destabilizing effects that repealing the ACA would have for these children. Thus claims data represent an important source of information that public health researchers need to consider in order to continue to create evidence that supports policymakers and public health practice.
